Since finishing my PhD I've been faced with a dilemma. In a nutshell, having come across a (somewhat serendipitous) observation in my PhD studies, should I publish it? I decided to publish, and it was both an editor's pick and is now regarded by the journal as 'highly accessed' (the importance and possibly ephemeral nature of such labels is a completely different discussion). That implies it was worthwhile, but was it?
The study revolved around an observation in BHK (hamster) cells infected with Bluetongue virus (BTV). The cells looked very strange: rounded and with condensed DNA/chromosomes in a pattern suggestive of some stage in mitosis, albeit a rather odd looking mitosis. To try and see what's going on, we used confocal microscopy with a panel of antibodies to look at the status of various parts of the cell division machinery. In brief, we found that the centrosome, a major orchestrator of mitosis, was severely disrupted. Co-incidence or not, the BTV protein non-structural protein NS1 also located in the region.
Something that was conspicuous was the association of the viral NS2 protein with the condensed chromosomes. When we took a series of images in the z plane and analysed them it became clear that NS2 appeared to be associated with the kinetochore. Combined with the observation of its location on microtubules, it is conceivable that NS2 may be a microtubule cargo molecule (or interacting with one) that obscures the kinetochore during the initial stages of mitosis. As the microtubules polymerise though the cell, the tips don't find the kinetochore, resulting in faulty mitosis. Many viral proteins use microtubules to get around and, based on other viruses, the dynein/dynactin complex would be an interesting place to start looking for a protein that interacts with NS2.
To look at whether NS2 alone is capable of inducing the aberrent mitosis, we transfected cells with plasmids encoding the protein. When looked at from a confocal perspective, the transfected cells appeared to reflect the phenotype seen with virus infection. When a GFP-tagged version of NS2 was used in live cell imaging, we found that the cells were less likely to complete mitosis correctly, spent longer in mitosis, and resulted in an increased level of binucleated cells.
 |
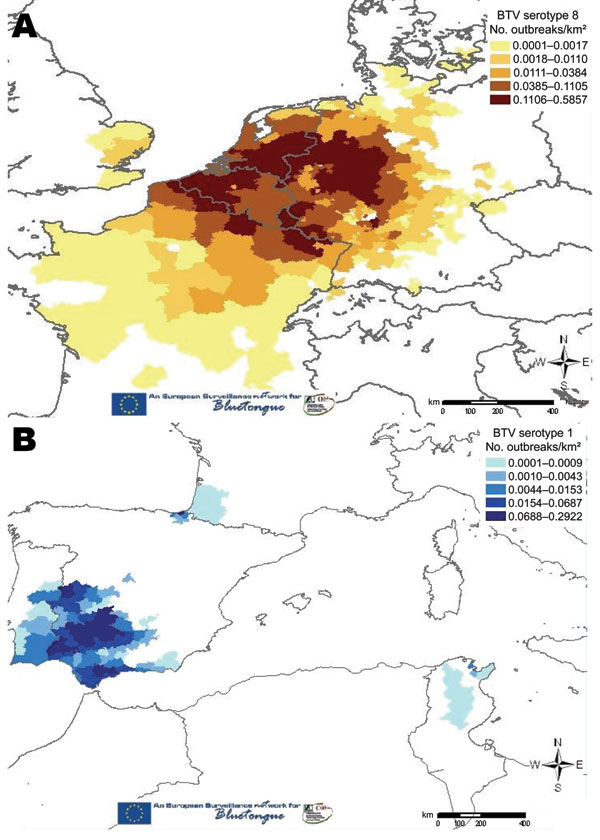
| A-D. Different BTV serotypes (16, 1 and 8) induce aberrent mitoses (although BTV-16v induces the most). Different cell types can also be affected, although BHK cells appeared to be the most susceptible. |
 |
| A. NS2 expressed from a plasmid locates to microtubules (red). B. Z stack images reveal NS2 located at positions suggestive of the chromosome centromeres. C and D. Expression of NS2 from a plasmid recreates the aberrent mitotic phenotype. |
To look at whether NS2 alone is capable of inducing the aberrent mitosis, we transfected cells with plasmids encoding the protein. When looked at from a confocal perspective, the transfected cells appeared to reflect the phenotype seen with virus infection. When a GFP-tagged version of NS2 was used in live cell imaging, we found that the cells were less likely to complete mitosis correctly, spent longer in mitosis, and resulted in an increased level of binucleated cells.
 |
| Transfecting HeLA cells with a palsmid expressing a GFP-tagged version of BTV NS2 resulted in a longer time spent in mitosis, a reduced level of successful mitosis, and binucleation. |
So, to the options.
1) don't publish. At the end of the day it's just an observation; I have not elucidated an exact mechanism and nailed down a precise protein, as would be expected for a publication in a journal of greater 'impact'. Not taking the story to an end, followed by publishing in a prestigious journal might be viewed as poor science by some.
2) publish. Many would argue that publishing information, regardless of how seemingly insignificant, is important and, arguably, a necessity based on the fact that it is being funded by the public.
I published. Partly for the reasons outlined in scenario 2, but also because the study was at a point where other people had contributed work, in which case it would not be fair for them to have done this work only for me not to publish. Of course, continuing the project to the end would have been my (and my collaborators') preferred option, but time ran out. As it stands, this observation is in the public domain for all to see, with the option of progressing it further to try and unravel what's happening.
Should I have published? I'm satisfied that I did, but it once again highlights the question of how many other such observations are languishing in abandoned lab books around the world.
Andrew E Shaw, Anke Brüning-Richardson, Ewan E Morrison, Jacquelyn Bond, Jennifer Simpson, Natalie Ross-Smith, Oya Alpar, Peter PC Mertens and Paul Monaghan (2013). Bluetongue virus infection induces aberrant mitosis in mammalian cells Virology Journal DOI: 10.1186/1743-422X-10-319
Should I have published? I'm satisfied that I did, but it once again highlights the question of how many other such observations are languishing in abandoned lab books around the world.