In recent years there seems to have been a resurgence in Bunyaviruses. There are always incidences of certain members, for example there are thousands of cases of hantavirus each year, as well as the sporadic cases of Crimean-Congo hemorrhagic fever virus. On the other hand there are the new emergents. In Europe, the most dramatic and devastating (at least in animals) has been Schmallenberg virus, which will no doubt now be familiar to more or less all cattle and sheep farmers.
As far as 'human' viruses are concerned, there have been a couple of highly related viruses: one in the Far East, and one the US. Severe fever with thrombocytopoenia syndrome virus (SFTSV) emerged in China in 2009, and was isolated from one of a series of patients with hemorrhagic fever. The virus from the US is Heartland virus (HV), and was isolated in 2009 from two cases in Missouri. The last few weeks have seen the second death in the US from Heatland virus, this time in Oaklahoma.
SFTSV and HV are both members of the phlebovirus genus of the Bunyaviridae. Rift valley fever virus (RVFV), currently one of the great fears for Europe, is also a member of this genus and is spread by mosquitoes. However, unlike RVFV, both SFTSV and HV are associated with ixoid and lone star ticks respectively.
| Distribution of the Lone Star tick in the US. |
Now a paper has been published describing another tick-borne phlebovirus, named Hunter Island Group virus (HIGV, after the location from which the ticks were sampled), this time from ticks associated with shy albatrosses on an island near Tasmania. Initially an aetiological agent couldn't be found; likely viruses such as Newcastle's disease virus and avian influenza were eliminated as likely causes. Although electron micrographs indicated a virus with morphology suggestive of a bunyavirus, antibody and PCR assays still failed to find a virus.
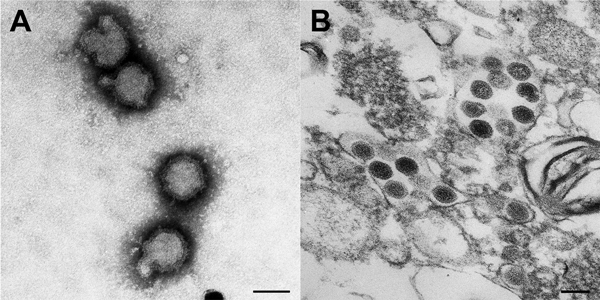 |
| Electron micrograph images of negatively stained virions (A) and thin sections of vero cell cultures (B). source |
Several years later they performed deep sequencing on infected cultures. Although the nucleotide sequences failed to match with anything close, blast searches using the protein sequence revealed similarity with SFTSV. With the foundations of the sequence now known the remaining sequence was filled in, allowing an analysis using the whole genome, as well as the design of molecular assays for the specific detection of HIGV. Perhaps unsurprisingly considering the results from the deep sequencing, the viruses fit into the bunyavirus clade next to SFTSV and Heartland virus.
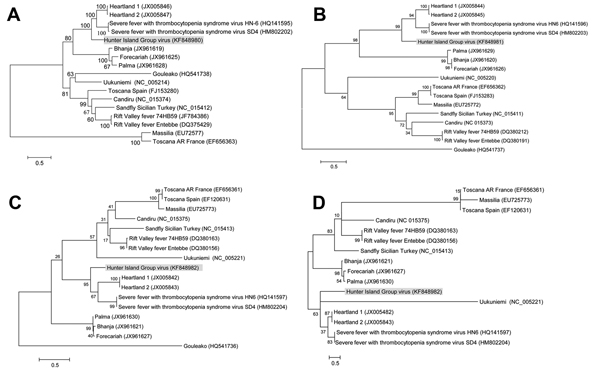 |
| HIGV: phylogenetic trees (amino acid sequence) of the viral polymerase (A), glycoprotein (B), nucleocapsid (C) and NSs (D). source |
As the ticks were associated with healthy as well as diseased birds, it was suspected that HIGV wasn't the cause of the outbreak among the shy albatrosses, something which was confirmed when the birds were tested for antibodies against, or the genome of, HIGV.
Richard Elliott, a well known figure in the bunyavirus world, says the discovery of this virus wasn't a surprise, and in a way was predicted. The simple truth is that if the ticks are there, then the viruses are there.
Discussing tick viruses with anyone always seems to leave one unanswered question; what is it that's so repulsive about ticks?
Wang J, Selleck P, Yu M, Ha W, Rootes C, Gales R, Wise T, Crameri S, Chen H, Broz I, Hyatt A, Woods R, Meehan B, McCullough S, & Wang LF (2014). Novel phlebovirus with zoonotic potential isolated from ticks, australia. Emerging infectious diseases, 20 (6), 1040-3 PMID: 24856477


